What does it mean that the WHO declared mpox a global public health emergency?
Written by ABC Audio ALL RIGHTS RESERVED on August 15, 2024
(NEW YORK) — The spread of a newer strain of mpox in Africa led the World Health Organization (WHO) to declare the disease a public health emergency of international concern (PHEIC) on Wednesday.
This newer strain is believed to be behind an outbreak in the Democratic Republic of the Congo (DRC) with more than 14,000 cases — mostly among children — and more than 500 deaths, and has been detected in neighboring countries that had never reported countries of mpox before.
On Thursday, Sweden became the first nation outside of the African continent to report a case of the newer strain of mpox, according to the country’s public health agency.
Cases of other strains, or clades, of mpox have popped up in other countries. In the U.S., there are more than 1,600 cases reported this year so far, more than twice the number seen at this time last year but not as many as seen during the outbreak in 2022-23.
“It’s clear that a coordinated international response is essential to stop these outbreaks and save lives,” said WHO Director-General Dr. Tedros Adhanom Ghebreyesus during a media briefing on Wednesday.
Experts told ABC News that by declaring a PHEIC, the WHO can help more countries collaborate by sharing data, allocating resources and helping make vaccines more readily available.
What is a PHEIC?
A PHEIC is defined as “an extraordinary event which is determined to constitute a public health risk to other States through the international spread of disease and to potentially require a coordinated international response,” by the International Health Regulations.
To be considered a PHEIC, the condition is considered, serious, sudden, unusual or unexpected; has implications for public health beyond where the place it originates; and has the potential to require immediate international action, according to the WHO.
“This is really [the WHO’s] highest level of alert,” Thomas Duszynski, director of epidemiology education at Indiana University’s Fairbanks School of Public Health, told ABC News.
“This means that this particular virus, or the mpox virus, and the illnesses that it causes, has reached a level that is now at a much higher rate than it should be, than when we see like in a normal year, as well as it’s starting to spill outside of the country of the Democratic Republic of Congo, which means that we have to get our arms around it and try and contain it,” he said.
A PHEIC was last declared for mpox during the outbreak in 2022-23, but this current outbreak is different because it involves a clade called clade Ib that seems to spread more quickly and has a higher mortality rate, Duszynski said.
What becomes available when a PHEIC is declared?
Emily Smith, an associate professor in the Department of Global Health at George Washington University’s Milken Institute School of Public Health, said declaring a PHEIC can help galvanize collaboration and mobilize resources.
“Collaboration can be really important in terms of sharing data from different surveillance systems or even things like genomic sequences, so we can understand how different cases are related to each other,” she told ABC News.
On the mobilizing resources front, Tedros said during the media briefing on Wednesday that WHO had released $1.5 million in contingency funds and planned to release more soon. The WHO’s regional response plan — including support surveillance and preparedness and response activities — will cost $15 million.
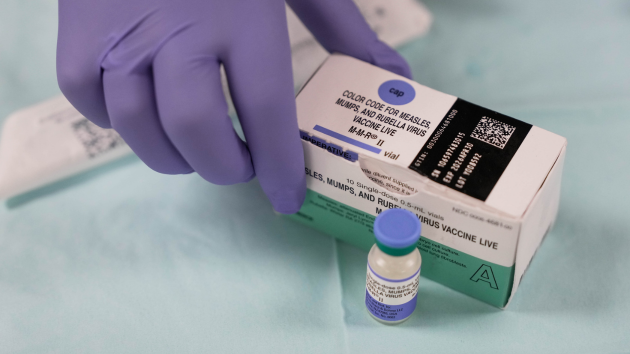
Additionally, last week, the WHO triggered the process to begin allowing mpox vaccines to go through the process for emergency use listing, similar to what was seen with the COVID-19 vaccine during the pandemic.
The PHEIC will also allow vaccines to be sent to other affected countries more quickly than they might have been without an emergency declaration, Duszynski said.
“In the Democratic Republic of Congo, their access to the impact vaccine is limited,” he said. “So, for example, the U.S. has dedicated 50,000 doses of that vaccine for the Democratic Republic of Congo, so that that’s part of that cooperation of not only sending, knowledge and science and research, but also aid, in the sense of vaccines.”
“We could also send personnel, such as epidemiologists, to help with the investigation and to help identify those who are ill and put some isolation and quarantine around those individuals to keep this virus from spreading,” Duszynski added.
What should the public do?
The experts said the best thing to do is to get vaccinated if you are a high-risk individual.
Currently, the JYNNEOS vaccine, a two-dose vaccine approved by the Food and Drug Administration to prevent smallpox and mpox, is the only vaccine being used in the United States to prevent mpox. Data from Africa has shown two doses of JYNNEOS are at least 85% effective in preventing mpox infection.
High-risk individuals include those who are immunocompromised, suffer from chronic diseases, or have a history of eczema, which causes breaks in the skin and can lead to mpox transmission.
Smith said other high-risk individuals include gay, bisexual or men who have sex with men — a group that was most affected during the 2022-23 outbreak — should get vaccinated.
She said that anyone who has only received their first dose should be sure to get their second dose.
“Just be aware if you or anyone you know, or your family, experiences lesions, skin lesions or genital lesions,” Smith added. “[You] definitely want to contact your doctor. We do have treatment options available in the U.S.”
Both Smith and Duszynski reiterated the Centers for Disease Control and Prevention’s warning that the general public is at low risk from the type of mpox circulating in the DRC.
Copyright © 2024, ABC Audio. All rights reserved.